Gastric Sleeve Surgery
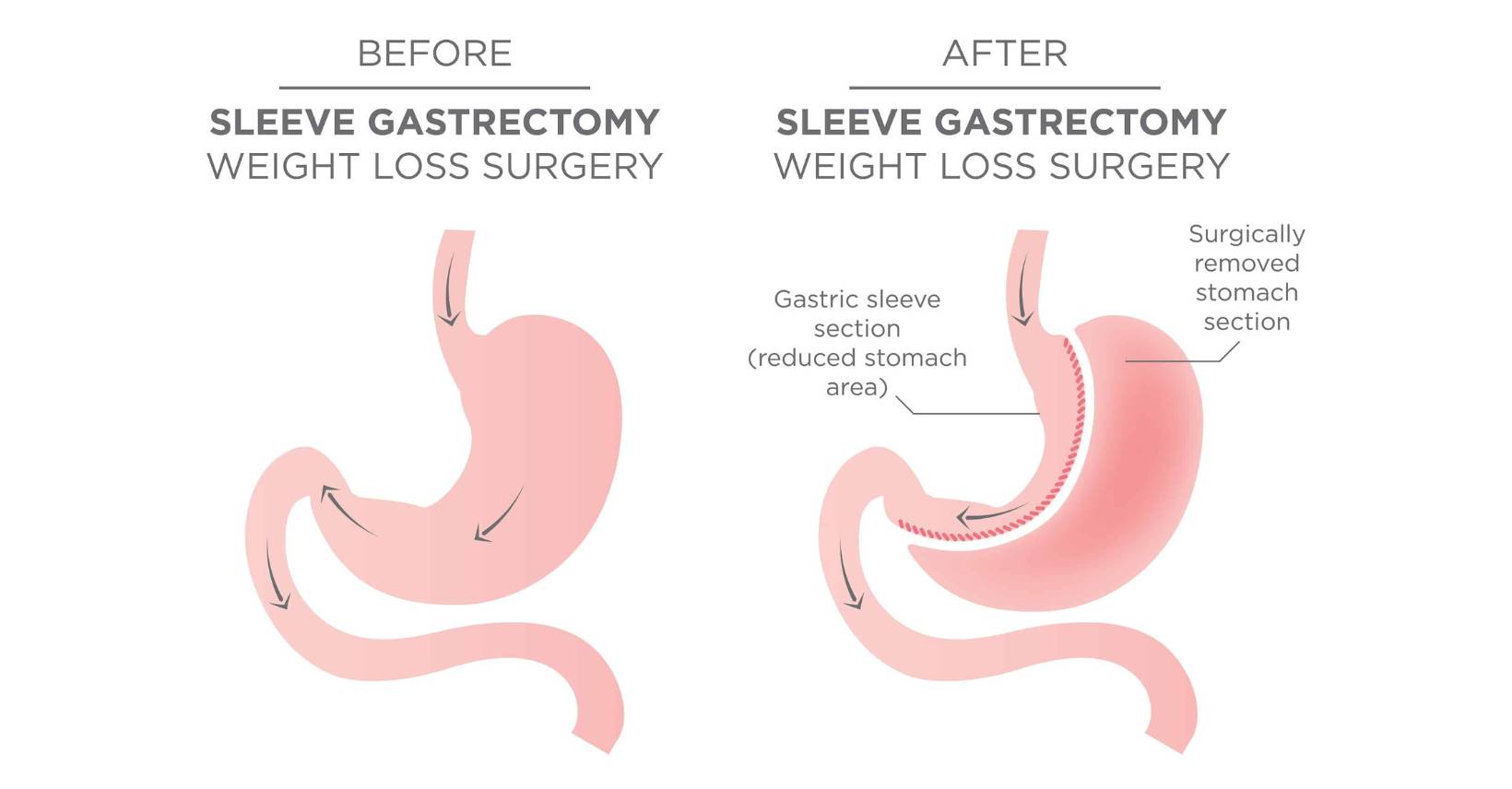
During gastric sleeve surgery, a big part of the stomach is removed. This leaves behind a smaller stomach that looks like a banana or a sleeve. This makes the stomach smaller, which makes you feel full after eating less, which leads to weight loss in over time.
How to do it:
Preparation: Before the surgery, the patient goes through a full evaluation, which may include a review of their medical history, a physical exam, blood tests, and possibly a psychological evaluation. It’s important to make sure that the patient is a good fit for surgery and that they understand what will happen.
Surgery: The surgery is usually done while the patient is asleep. Laparoscopic techniques are often used to do it. These involve making a few small cuts in the abdomen and using a camera and surgical tools to do the treatment. The surgeon takes out about 75–80% of the stomach, leaving behind a stomach in the shape of a thin sleeve.
The surgery usually takes between 1 and 2 hours, but the exact time can change from person to person.
Who qualifies for gastric sleeve surgery?
Generally, these people are good candidates for gastric sleeve surgery:
1- BMI Criteria: Most people who get gastric sleeve surgery have a body mass index (BMI) that falls into one of these ranges:
- If your BMI is 40 or higher, you are thought to be very obese.
- People with a BMI between 35 and 39.9 may be taken into account if they have health problems linked to obesity, such as type 2 diabetes, high blood pressure, sleep apnea, or joint problems.
2- Attempts to lose weight in the past: Good candidates have tried to lose weight without surgery, such as through diet and exercise, but haven’t been able to do so in a way that is important and long-lasting.
3- Health Conditions: People should have health problems that are caused or made worse by their weight that may get better if they lose weight. Some of these problems are type 2 diabetes, high blood pressure, sleep apnea, and more.
4- Motivation and commitment: Candidates should be ready to make big changes in their lives after surgery, like eating healthier, working out regularly, and getting long-term care.
5- Psychological exam: Candidates go through a psychological exam to make sure they have realistic goals and are mentally ready for the changes that come with surgery and weight loss.
6- Age and medical history: Age is not the only factor, but most possibilities are between the ages of 18 and 65. A detailed look at the patient’s medical history is done to find any problems or factors that could affect how the surgery goes.
7- Absence of Certain Medical Conditions: People who want to get surgery shouldn’t have certain medical conditions that could make surgery more dangerous.
8- Willingness to follow instructions: Successful candidates are ready to follow pre-operative and post-operative instructions, such as what to eat, how much exercise to do, and when to come back for checkups.
9- Realistic Expectations: People who want to have the surgery should have realistic expectations about how it will turn out, and they should know that it is a tool to help them lose weight, but that they will still have to make changes to their lifestyle.
It’s important to remember that everyone’s situation is different, and choices about who can have surgery are made case by case. To find out if gastric sleeve surgery is the right choice for a certain person, a healthcare team needs to do a thorough review. There are risks and possible problems with the surgery, so the benefits and risks should be talked about in detail before deciding.
Step-by-step explanation of the Gastric Sleeve Operation:

1. Surgical Procedure:
- Anesthesia: The surgical process is carried out while the patient is under general anesthesia, which means that they are put to sleep and are not in any discomfort during the operation.
Incisions: The surgeon will make a few different, relatively minor incisions in the patient’s belly. These incisions are typically between a quarter and a half of an inch in length.
Endoscopic Approach: The procedure is typically performed laparoscopically, which means that it is carried out with the assistance of a laparoscope (a thin, flexible tube equipped with a camera and light) and other specialized surgical instruments that are inserted through the incisions.
Stomach Division: The stomach is precisely divided vertically by the surgeon, resulting in the shape of a tube or sleeve that is narrower at the top and wider at the bottom. The section of the stomach that was removed is no longer present in the body in any capacity.
Stapling: involves dividing the stomach and then using surgical staples to seal it off. The staple line assists in preventing leaking and ensures that the remaining stomach keeps its new form by providing structural support.
2. Stomach Size Reduction:
The fundus, which is connected with the synthesis of hormones that regulate appetite, such as ghrelin, is found in the region of the stomach that is removed after surgery. By eliminating this component, the amount of ghrelin that is produced is diminished, which in turn results in a smaller hunger.
When compared to the capacity of the old stomach, the new stomach sleeve has a capacity that is noticeably lower. Because of this, the patient is only able to consume a certain amount of food at one sitting.
3. Hospital Stay and Recovery:
The majority of surgeons recommend that their patients remain in the hospital for one to two days following surgery for monitoring and pain management.
Recovery times can vary, but for the most part, patients are able to resume simpler tasks and go back to work within two to four weeks of having surgery.
The first few days after surgery are typically marked by increased levels of pain and discomfort, although these side effects typically decrease over time.
4. Post-Operative Diet:
Patients follow to a planned post-operative diet routine that begins with clear liquids, moves on to pureed foods, and then transitions them into soft solids.
The goal is to avoid issues such as vomiting or straining of the stomach while allowing the stomach to heal and acclimatize to its new size.
5. Long-Term Changes in Lifestyle:
Adopting and sustaining a healthy lifestyle is necessary for the surgery’s success. Patients must commit to permanent dietary and physical activity modifications.
Patients must ingest smaller portions and thoroughly chew their food to avoid discomfort or complications.
Regular physical activity is crucial for weight loss, muscle maintenance, and overall health.
6. Follow-Up Care:
Follow-up meetings with physicians are required on a regular basis to evaluate progress, address any issues or concerns, and change food and lifestyle recommendations as needed.
Blood tests are performed to check nutritional levels and ensure that patients do not become deficient.
7. Weight Loss and Health Benefits:
The first 12 to 18 months following gastric sleeve surgery are often associated with significant weight loss for the majority of patients. The amount of weight lost may differ from person to person due to several reasons.
A significant number of individuals have obesity-related health issues, such as type 2 diabetes, hypertension, sleep apnea, and joint pain, which improve or go away completely after treatment.
Gastric Sleeve Diet:

What can you eat after Gastric Sleeve Surgery?
Patients who have undergone gastric sleeve surgery are required to adhere to a diet progression that has been meticulously prepared in order to give their stomach time to heal and adjust to its new, smaller size. The post-operative diet will normally begin with liquids and then progressively develop to include more solid foods as time passes. The following is a summary in broad strokes of the numerous kinds of foods that patients can eat at various phases of their recovery:
Clear Liquid Diet (Week 1-2):
Clear liquids include things like water, clear broth, sugar-free gelatin, and popsicles that don’t have any added sugar.
The need of maintaining adequate hydration and placing as little strain as possible on the stomach that is recovering is emphasized.
To avoid taking in an excessive amount of air while drinking liquids, it is essential to sip them slowly and refrain from using straws.
Full Liquid Diet (Week 2-3):
Full liquids are denser than clear liquids and include things like protein drinks, low-fat yogurt, and thin soups. Clear liquids do not have any solid particles suspended in them.
This stage allows for a little greater intake of both nutrients and protein.
Pick beverages that are low in sugar and fat if you want to stay healthy.
Pureed Diet (Week 3-4):
The foods are blended till they have a consistency comparable to that of baby food.
Pureed vegetables, lean forms of protein (chicken, turkey, or fish), and cottage cheese with a reduced amount of fat are some examples.
Because of the importance of texture, you should steer clear of foods that have chunks or solid pieces.
Soft Diet (Week 4-5):
The first foods that are consumed are those that are soft and easy to chew as well as digest.
Some examples of this type of food are vegetables that have been cooked, fruits that have been softened, eggs that have been scrambled, and finely ground meats.
Continue to stay away from meals that are tough or fibrous, as they may be difficult to digest.
Transition to Solid Foods (Week 5+):
Start with things that are easily chewed, including soft proteins and cooked vegetables, and work your way up to larger portions of solid foods.
It is important to chew food completely in order to avoid discomfort and facilitate digestion.
While you gradually introduce new foods into your diet and pay attention to how your stomach reacts, you can expect to feel better.
General Guidelines:
- Ensure that the majority of your protein intake comes from lean sources such as chicken, turkey, fish, eggs, and low-fat dairy products.
- As soon as you receive clearance from your healthcare professional, begin including a wide variety of fruits and vegetables into your diet. Whole grains are the best choice if you’re looking for fiber and lasting energy.
- Foods that are heavy in sugar and fat should be avoided because they might cause discomfort and make it more difficult to lose weight.
- To avoid overeating, it is important to pay attention to portion sizes and to eat slowly.
Keep in mind that the healing process for each patient can be unique, and the evolution of the specific diet may change depending on the individual’s requirements and the recommendations of the healthcare team. It is essential to adhere to the advice that have been given to you by your healthcare professional or nutritionist in order to facilitate a speedy recovery and get the most out of the surgical procedure. In addition, continuing nutritional support and follow-up appointments are essential in order to address any difficulties and make any adjustments.
Risks and Complications of Gastric Sleeve
While gastric sleeve surgery is generally considered safe, it carries risks similar to any major surgery, such as bleeding, infection, blood clots, or adverse reactions to anesthesia.
As mentioned before, there is a risk of leakage from the staple line, which can lead to infection or other complications.
Send Us A Message
Useful Links

Mesotherapy Hair Loss Treatment
Mesotherapy is a medical procedure that includes injecting a mixture of vitamins, minerals, medicines, and other things directly into the scalp to treat hair loss. It is generally used as a non-surgical treatment for hair loss and is said to encourage hair growth and enhance scalp health. A healthcare expert

Platelet-Rich Plasma (PRP)
Platelet-rich plasma (PRP) therapy is a medical procedure that has been used to treat a variety of conditions, including hair loss. PRP is made up of concentrated platelets and growth factors derived from the patient’s own blood. These growth factors are thought to encourage hair development and increase the thickness

Dental Implants Surgery
Dental implants have been demonstrated to be successful in helping people with tooth loss improve their quality of life. Successful tooth replacement can enhance and restore the patient’s quality of life by improving the bite and providing a better eating experience, and it can also last a long time. Dental